
Access to reproductive health care in the Interior continues to come under the spotlight as local clinics like the Thompson Region Family Obstetrics group struggle to meet demand. While other prenatal services aim to fill in some of the gaps, services remain hard to access, including abortion care — an integral part of prenatal health care.
Experts interviewed by The Wren say access to abortion services, while available, is limited and in some cases patients must drive to larger urban centres like Kelowna or Vancouver to access.
Sage Thomas, who is currently both a midwifery student at the University of British Columbia and a parent, says the expansion of existing reproductive health care services in Kamloops would go a long way.
The 37-year-old believes that barriers to accessing abortion care in the Interior exist due to the overall shortage of healthcare professionals for individuals in the community.
“We’re in the Interior, at a place where people have limited access to prenatal care, so when we think about abortion care, there’s even more limited care options,” says Thomas. “Unless you’re in a big city like Vancouver, you often don’t even know where to go to get you to where you need to be.”
To improve access, experts say it’s time to involve more health professionals like midwives and paraprofessionals in abortion care. Involving more practitioners and clinicians in this aspect of prenatal care could not only take the burden off other healthcare professionals but also help combat the stigma that, decades after legalization, continues to stir division and shame.
What abortion services are available locally?
The Interior Health Authority (IHA) declined The Wren’s request for a phone interview regarding abortion services in Kamloops, citing concerns for the privacy, safety and security of both its staff and patients. While they would not provide specific details about the locations of abortion care, abortion is funded as a “core health service” by the province, IHA spokesperson Jennie Bui tells The Wren via email. This means pregnant people in B.C. can access care through abortion clinics as well as some general practitioners, nurse practitioners, gynecologists and hospitals, including Royal Inland Hospital.
While the IHA is one of the largest health jurisdictions in the province, just three clinics provide surgical abortions (in Kelowna, Nelson and Cranbrook) according to the health authority website. Surgical abortions, often involving a technique called aspiration, may be required for a variety of reasons, such as a later-term pregnancy or miscarriage.
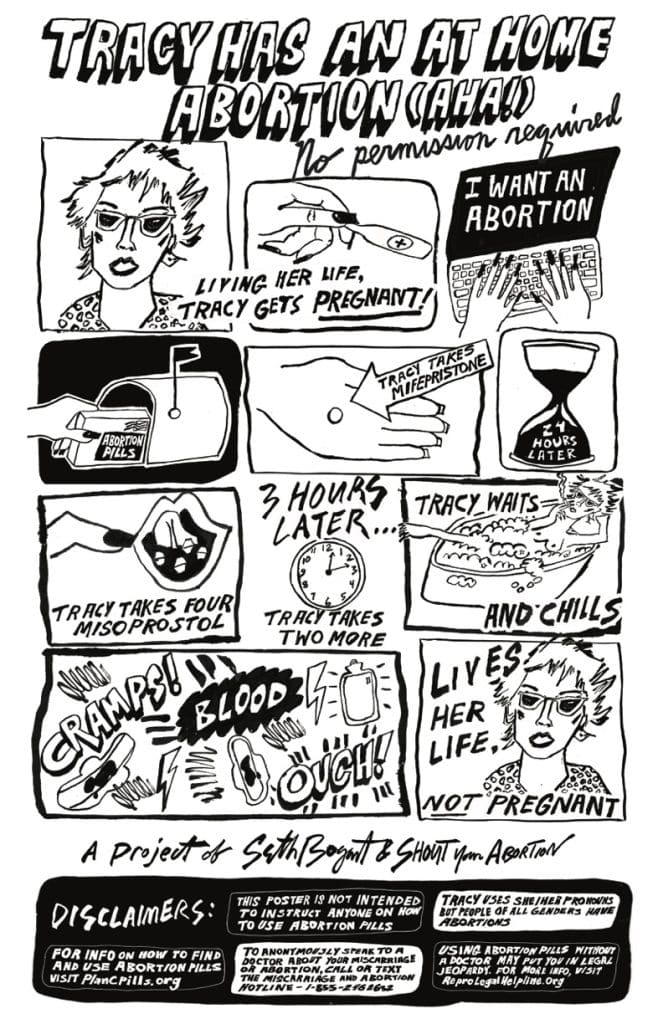
Medical abortion, a more accessible form of abortion care involving a combination of medications (mifepristone and misoprostol) taken under the supervision of a doctor, is available at the Kamloops STEPS Women’s and Sexual Health Clinic for up to 10 weeks from a person’s last menstrual period.
For a person who is at a later term or at-risk of complications such as excessive bleeding, hospital services may be required. But the hospital can be harder to access for people in growing communities like Kamloops.
And while most abortion care providers in B.C. require counselling to ensure the individual is independently sure of their decision, informed of the risks and has access to contraceptives, abortion-related counselling from a trained psychologist is harder to access in Kamloops, according to multiple sources interviewed by The Wren.
Interior Health says on its website that abortion care can be expedited if a health provider orders an urgent ultrasound, but delays in booking or referrals can mean the difference between what type and where a pregnant person can access services. As the process of human development continues, and gestational age increases, the number of healthcare providers who are willing to provide later-term abortion care significantly decreases, according to Action Canada, which provides education and advocacy for sexual health.
In many communities across the country, including Kamloops, abortion care is only available until approximately 14 weeks, resulting in the need to travel to access later-term abortion care. Though less common, a later-term abortion may be required to protect a patient’s health or because of fetal abnormalities, some of which may only show up during second-trimester screening, between 13 to 26 weeks.
Meanwhile, procedures occurring later in the pregnancy are often scheduled over several days, which requires more time off from work, childcare arrangements for parents and many other logistical or financial challenges for those in need.
Action Canada reports a “sharp increase” in people seeking later-term abortions since 2020, in part because of the long wait times to access abortion care and these services remaining largely in urban centres.
Why is abortion care hard to access?
One in three people who can get pregnant will have an abortion during their lifetime, and about half of the pregnancies every year are unplanned, according to Action Canada. Most people who get abortions already have one child, according to the Guttmacher Institute, a reproductive health research organisation.
While accessing abortion care was fully decriminalised more than 30 years ago, in 1988, each province and territory has continuously reported barriers to pregnant people accessing abortion and post-abortion care.
For instance, a quick Google search for local abortion services usually brings up crisis pregnancy centres — non-medical facilities known to operate under the belief that abortions should be discouraged. That’s because these centres outnumber medical facilities that provide abortion health care.
Abortion Rights Coalition of Canada has found 23 crisis pregnancy centres in B.C., while the Interior Health website lists 12 options for abortion care across the province.
These anti-choice clinics are in some cases providing misinformation to individuals who do not wish to be pregnant.
“It can be really tough (to detect and avoid what are known as fake abortion clinics) because they’ve been really savvy at adopting pro-choice language,” says National Abortion Federation (NAF) Canada executive director Jill Doctoroff. “Some clues are things like post-abortion syndrome, which doesn’t exist, it’s a made-up condition.”
The lack of access to safe, timely and elective abortion and post-abortion care has been associated with longstanding risks for the childbearing population and the healthcare providers equipped to deal with it due to systemic issues like sexism, colonialism, poverty, racism and ableism.
“Abortion care is health care, but it’s different because of the stigma that comes with it,” Doctoroff says.
Who is left behind when it comes to abortion care in Kamloops?
Travelling long distances to access health care can be especially challenging for those in need of care due to time away from work, logistics like child care and privacy.
“If you’re going away for a longer period of time, it’s going to compromise your privacy and the burden of travelling is pretty significant for many people, let alone for people with immigrant status who can’t travel as easily,” Doctoroff explains.
For Laura Salamanca, director of health promotion for Action Canada, people in need of support with access to abortion care are often facing barriers that have to do with immigration status and language.
“Or they might be a migrant worker who’s here and their employer is restricting their movement, but also they don’t have permanent residency status, and so they [might not be] covered under provincial coverage,” she adds.
“Or they might be somebody who’s homeless, who doesn’t have access to their ID or access to a space to go through the process of getting medical care.”
Cases like these inform Action Canada’s efforts to improve access to comprehensive contraception coverage for all people living in Canada.
People living outside of their home province may also face gaps in coverage for abortion care. Most people can access surgical and medical abortions for free in B.C. and non-residents may be covered by Non-Insured Health Benefits and the Interim Federal Health Plan, excluding the territory of Nunavut. Hospitals are anecdotally more equipped to field requests for interprovincial billing when abortion care is required in another province.
However, medical abortion is not covered by interprovincial billing for those who need to access care outside of their home provinces.
As of last year, British Columbians have access to free prescription contraception, which can also be accessed at local pharmacies if people do not have a family doctor, but this excludes the medication for interprovincial medical abortions, according to Action Canada.
Doctoroff has been accepting donations for roughly a decade now to allow uninsured individuals who need to travel to access abortion care. Doctoroff emphasised the importance of this funding model for individuals with immigration status, permanent resident status, changed visas, pre-refugee status (for those who have not yet applied), undocumented immigrants and Canadians who relocate from one province to another.
Calling for culturally safe health care
Sage Thomas, a midwifery student at the University of British Columbia, indicated there’s a lack of pre-counselling to ensure abortion care is the right choice for people in Kamloops, whether they choose to have an abortion or not.
While Interior Health has an Indigenous Patient Navigator Service for Indigenous individuals, this is especially true for Indigenous people who are seeking culturally safe and relevant pre-counselling and health care.
Thomas added the BC Aboriginal Doula Grant Program provides funding for a support person at an abortion procedure, but felt it was an “extremely underutilised service” due to lack of knowledge about the program and time constraints related to gestational stage.
“I think people should have the information,” Thomas says.
She feels it’s essential for healthcare providers to have direct conversations with their clients to ask how best to support Indigenous families from a cultural perspective so that they feel safe utilising health services in the hospital and in the community.
“Each individual Indigenous family or person are the ones who can identify what cultural safety looks like for them,” she explains.
The First Nations Health Authority (FNHA) explains cultural safety is an outcome derived from respectful engagement that strives to address power imbalances that are inherent in the healthcare system.
“It’s important for people to have access to that information quickly and feel comfortable talking about it,” Thomas says. “There are some places (here) that are more pro-life, and they’re possibly going to influence what that choice may look like.”
Indigenous people need support throughout their prenatal experience, Thomas adds, recalling a family who recently reported feeling unsafe navigating pregnancy complications at the Royal Inland Hospital.
“Most folks who are going into health care facilities are going to feel scared, so I think when health care providers want to provide culturally safe care, they need to understand what that looks like.”

Midwives call for increased scope of practice in BC
Ace Porter has been a practising midwife in Kamloops (Tk’emlúps) for the last nine years.
Her desire to support the community with reproductive health care has made her a strong voice and ally in the community.
“I think my interest is just more broadly in providing comprehensive reproductive health care to my clients as a midwife and finding that there are these areas of scope that prevent me effectively supporting my clients,” Porter says. “I’ve done the National Abortion Federation (NAF) training for terminations, which is all of the prescribing training and everything, so I actually have the knowledge I need to do this, but I don’t have the scope I need to do this.”
She tells The Wren it would be helpful if the midwifery practice in B.C. expanded its scope to include reproductive health care and justice rights for childbearing individuals to make accessing services simpler, and to assist with taking the burden off of other healthcare professionals in the community.
“I would like to see us, midwives, given prescribing rights (for medications like mifepristone/misoprostol to provide medical abortions) and access to NAF training,” Porter says. The Canadian Association of Midwives (CAM) supports Canadian midwives who already provide abortion and post-abortion care and midwives who are working to integrate this care into their practice today, but the means and education to provide abortion care differ across the nation.
“The idea when someone is having an abortion is to ensure people don’t have to go through that difficult decision again and we do try to make sure they have access to whatever kind of information required,” Porter says, while indicating the importance of preventative birth control options, like the pill or an IUD, without paying out of pocket.
“Abortion care access is really important health care. The more we can shine the spotlight on where we need to be with access, the better.”
Follow up could improve abortion care
The path to navigating the emotionally complex aftermath of an abortion, especially as hormones gradually return to their baseline, is an ambiguous one. There are no clear support groups and counselling options are very limited. Wild Roots Traditional Chinese Medicine and Acupuncture Clinic owner Andrea Hansen voiced a strong desire for the standard of prenatal care to include trauma-informed services for those accessing abortion care.
“Ultimately what I would like to see is the form of care put in place with a GP, a nurse practitioner, a midwife or someone like me where these are a part of the plan, and counselling, should be automatically provided to someone after an abortion,” Hansen says.
As a doctor of Traditional Chinese Medicine (TCM) and Acupuncture, her patients pay out of pocket or access services through their extended health benefits, although supplementary benefits are available for people on disability and income assistance.
She started practising in a Vancouver clinic after completing her studies several years ago with a focus on caring for people who were trying to get pregnant, stay pregnant and supporting them after a birth or a loss.
“During that time, I also had my own children, I’ve had my own experiences through reproductive health and all of those things and the importance and the richness of support that it offers,” Hansen says, stating that certain translators and authors influenced her practice in TCM.
“One of them in particular really focused on postpartum care and continually working with women struggling after they’ve had children,” she explains. “At any stage of pregnancy when there’s been a loss at any stage, there is a huge impact on [a] woman’s body or mind… whether the pregnancy is terminated or there’s a loss, the importance is the same.”
Hansen says without proper follow-up care, some individuals aren’t going to feel safe asking about ongoing physiological or emotional issues due to the polarising nature of abortion care.
“I would like to see a standard of care go deeper, whether it’s a couple of appointments put in place for follow-up care as a standard procedure,” she says. “I think because of the topic itself and how polarising it can be, it just doesn’t allow for a discussion that’s open which is needed, and it’s really too bad.”
There is a lot of focus in the acupuncture world on fertility to help women get pregnant, but the other perspective of that includes pregnancy loss whether that’s from an abortion, miscarriage or stillbirth. She encourages childbearing individuals to consider TCM as a form of post-abortion care.
“I think the primary thing that I offer is the benefit of post-abortion care as it pertains to Chinese medicine and acupuncture,” Hansen says, indicating that Chinese herbs, acupuncture, moxibustion and heat treatment are helpful forms of aftercare for someone experiencing a pregnancy loss.
“The support can be there but there’s so many people who never think of how they had an abortion and need some extra care. I hope people can access care a bit more. I support all bodies in all stages of their reproductive experiences, so acknowledging that kind of process in the body and the potential impact of it is so important.”
So do we. That’s why we spend more time, more money and place more care into reporting each story. Your financial contributions, big and small, make these stories possible. Will you become a monthly supporter today?
If you've read this far, you value in-depth community news





